Key Takeaways:
- Workflow Layer: Behavioral Healthcare Operations Software supports care delivery by managing intake, scheduling, documentation workflows, billing coordination, compliance, and reporting.
- Reduce Friction: Operational friction, not clinical skill, is a major source of clinician burnout, missed appointments, delayed access, and revenue leakage in behavioral health settings.
- Behavioral Fit: Behavioral healthcare requires flexible software that supports longitudinal care, group therapy, program-based treatment, and sensitive privacy requirements.
- RCM Alignment: Clean alignment between documentation and billing workflows helps reduce RCM issues and prevents clinicians from reworking notes after care delivery.
- Security Privacy: Security, privacy, and role-based access are foundational in behavioral healthcare operations software, not optional features.
- Clinician Input: Clinician involvement in software evaluation improves adoption, usability, and long-term value across behavioral health organizations.
Behavioral healthcare is deeply human work. Clinicians dedicate their time, expertise, and emotional energy to supporting individuals through some of the most complex health challenges. Yet behind every patient interaction lies an operational system that can either support care delivery or quietly undermine it.
Missed appointments, long intake cycles, fragmented documentation, billing confusion, and compliance pressure affect clinicians daily, even when they are not directly responsible for operations. As behavioral healthcare organizations grow and diversify their services, these challenges become harder to manage without the right digital foundation.
Behavioral healthcare solutions exist to bridge this gap. Not by replacing clinical judgment, but by creating an operational environment where clinicians can focus on care rather than administrative friction.
This guide is written for clinicians and healthcare domain professionals who want to understand how operations software fits into modern behavioral healthcare, what features matter most, and how to evaluate the right solution.
Understanding Behavioral Healthcare Operations Beyond Clinical Care
Healthcare software is often associated with Electronic Health Records and clinical documentation tools. While these systems are essential, they represent only one component of care delivery.
Behavioral healthcare operations include the processes that surround and enable clinical work, such as patient intake, scheduling, documentation workflows, billing coordination, compliance management, and reporting. These operational layers determine how smoothly care is delivered and how sustainable clinical programs remain over time.
Behavioral healthcare introduces unique complexities compared to other specialties. Care is frequently longitudinal rather than episodic. Treatment may include individual sessions, group therapy, intensive outpatient programs, residential care, and community-based services. Privacy requirements are more sensitive, and outcomes are not always captured through standardized clinical metrics.
Operations software designed for behavioral healthcare must balance structure and flexibility. It should support consistency while allowing care teams to adapt to individual and program-level needs.
Operational Challenges Clinicians Experience Every Day
Clinicians may not oversee operational systems directly, but they feel their impact every day. Several challenges consistently surface across behavioral health settings.

-
Intake And Access Delays
Patients often wait weeks between referral and their first appointment. Manual intake processes, incomplete documentation, and insurance verification delays create barriers to timely care and increase frustration for both patients and clinicians.
-
Scheduling Complexity
Behavioral healthcare scheduling goes beyond simple appointment booking. Balancing individual sessions, group therapy, shared spaces, and clinician availability requires coordination that many generic systems cannot support effectively.
-
Documentation Burden
Behavioral health documentation is detailed and time-consuming. When systems are fragmented or poorly designed, clinicians spend excessive time navigating workflows instead of focusing on patient interaction.
-
Billing-Related Friction
Documentation gaps and disconnected systems also contribute to behavioral health RCM challenges, where delays, rework, and denials affect financial stability and indirectly increase pressure on clinical teams. When documentation and billing systems are misaligned, clinicians are often asked to revisit notes or clarify details long after care has been delivered.
-
Limited Operational Visibility
Without access to clear operational insights, clinicians and leaders struggle to understand patient flow, workload distribution, and program performance. This limits improvement efforts and resource planning.
These challenges reflect system design gaps rather than individual performance issues.
Quick Stat:
One mental health clinic study reported a 9.7% no show rate and 17.3% cancellations (a combined 27%) during 2016 to 2017, with variation by patient group and clinician type. When scheduling systems do not actively support reminders, waitlists, and quick rebooking, these missed slots translate into lost access for patients and more disruption for clinicians.
What Is Behavioral Healthcare Operations Software?
Behavioral healthcare operations software is a digital platform designed to manage the non-clinical workflows that support care delivery. It coordinates people, processes, data, and compliance requirements across the organization.
Unlike generic healthcare management tools, this software is built around behavior-specific workflows. It accounts for group therapy structures, program-based care, sensitive privacy requirements, and long-term patient engagement.
It also differs from traditional EHR systems. While EHRs focus on clinical records, operations software connects intake, scheduling, documentation workflows, billing, compliance, and reporting into a unified operational layer.
The goal is not more technology, but better alignment between clinical care and organizational operations.
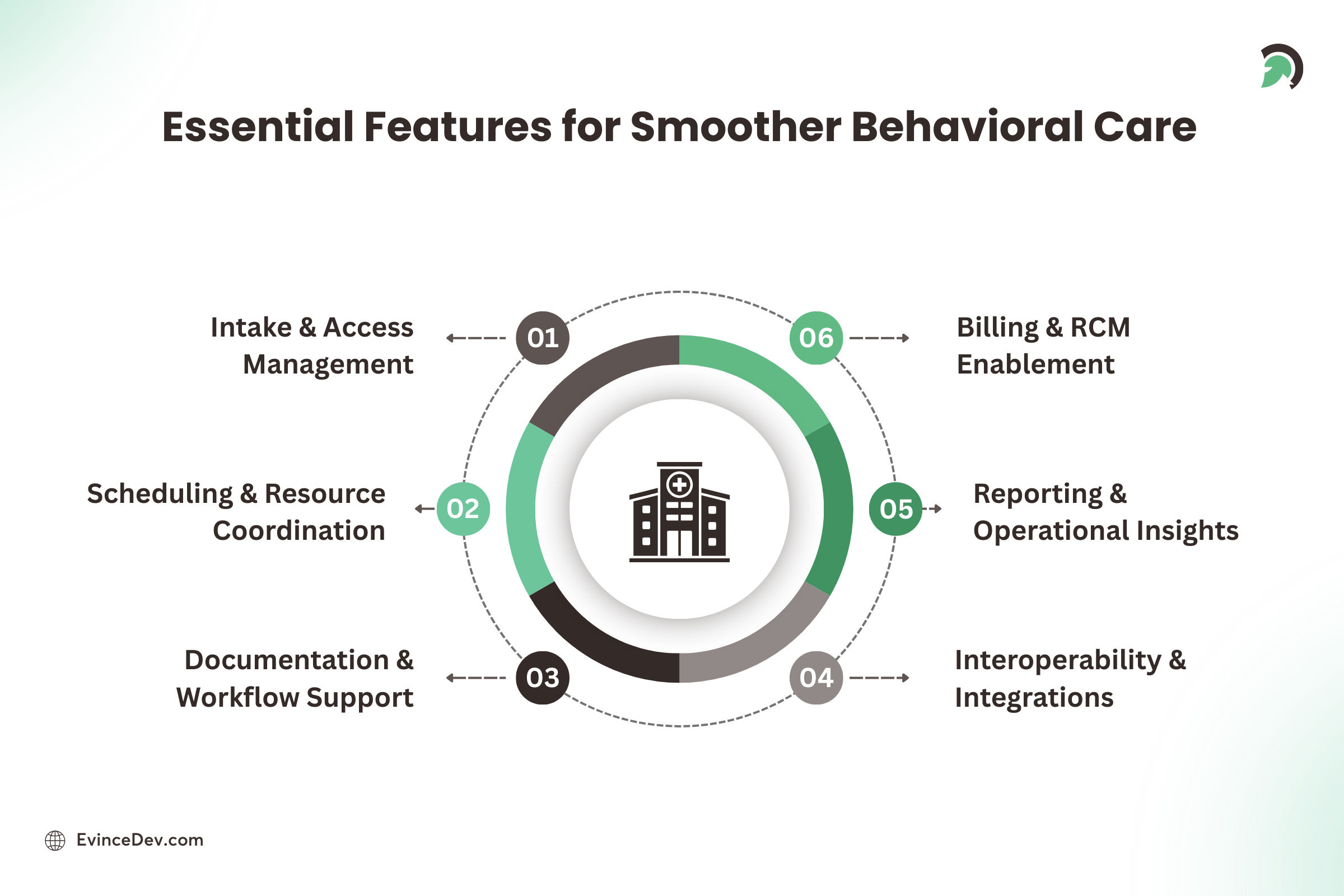
Core Features Clinicians And Healthcare Teams Should Look For
The most valuable features are those that reduce friction and support care delivery without adding cognitive load.
-
Patient Intake And Access Management
Effective intake establishes the foundation for the care journey. Operations software should support digital referrals, structured intake forms, eligibility verification workflows, and secure consent management. When intake processes are clear and efficient, clinicians can begin care with a better context and preparation. Secure messaging, appointment reminders, and digital forms strengthen behavioral health patient engagement while reducing administrative follow-ups for care teams.
-
Scheduling And Resource Coordination
Behavioral health scheduling requires more than calendar management. Software should support individual and group sessions, clinician availability, room and resource allocation, waitlist management, and automated reminders to reduce missed appointments. For residential and program-based settings, real-time capacity tracking and admissions workflows enable behavioral health bed management without relying on spreadsheets or manual updates.
-
Documentation And Workflow Support
Operations software should simplify documentation rather than increase workload. Features such as task reminders, incomplete note alerts, role-based access, and structured workflows help clinicians stay compliant without constant manual follow-up.
-
Billing And Revenue Cycle Enablement
Although billing teams handle claims, clinicians influence reimbursement through documentation quality. Operations software should enable clean handoffs between clinical documentation and billing workflows, surface issues early, and reduce rework. Modern platforms increasingly support Claims Automation for Behavioral Health Providers by reducing manual handoffs, catching documentation gaps early, and improving claim submission consistency.
-
Reporting And Operational Insights
Data should support decision making, not overwhelm users. Useful reporting includes utilization metrics, workload trends, program performance indicators, and operational summaries that healthcare leaders can act on.
Technical Foundations That Matter To Healthcare Professionals
Clinicians may not manage technology directly, but they rely on its reliability and integrity.
-
Security And Privacy By Design
Behavioral health data is highly sensitive. Software should incorporate strong access controls, audit trails, secure data storage, and privacy-aware workflow design as core elements rather than add-ons.
-
Interoperability And Integration
Operations software should integrate with existing EHR systems, billing platforms, telehealth tools, and reporting solutions. Integration reduces duplicate work and minimizes fragmented workflows.
-
Scalability And Flexibility
As organizations grow and care models evolve, software must adapt. Platforms should support multi-location operations, program expansion, and configurable workflows without major disruption.
-
Cloud-Based Reliability
Modern platforms leverage cloud infrastructure to deliver availability, performance, secure access, and continuous improvement without interrupting care delivery.
Quick Stat:
A 2024 KLAS Arch Collaborative interoperability report found that many healthcare organizations still report inconsistent data sharing and feel unable to meaningfully improve interoperability for clinicians and patients, despite progress connecting to exchanges and HIEs.
Compliance Considerations In Behavioral Healthcare Software
Compliance is closely tied to trust, patient safety, and organizational stability, especially in behavioral health, where data sensitivity is high. The right operations software should make compliance easier to follow in daily workflows, not something teams have to manage separately.
At a minimum, it should support:
Consent Management
- Secure capture and storage of patient consents
- Clear visibility into what information can be shared, and with whom
Role-Based Access Controls
- Restricting records and functions based on job role
- Limiting exposure to sensitive information while enabling coordinated care
Audit Readiness
- Audit trails that track access, edits, and key actions
- Structured documentation workflows that reduce missing or incomplete records
Regulatory And Payer Reporting
- Support for required reporting formats and operational metrics
- Easier documentation alignment for reviews, audits, and reimbursements
For clinicians, the goal is confidence and clarity: documentation should meet regulatory expectations and internal policies without adding unnecessary friction to clinical work.
How Clinicians And Healthcare Leaders Should Evaluate The Right Software?
Selecting operations software is a strategic decision that benefits from clinician involvement.
Key evaluation questions include:
- Does the software reflect real behavioral health workflows?
- Will it reduce administrative burden for clinicians?
- Is the user experience intuitive and practical?
- Can the platform adapt to evolving care models?
- Does the development partner demonstrate healthcare domain expertise?
The right solution should feel supportive rather than restrictive.
Who Benefits The Most From Behavioral Healthcare Operations Software?
Behavioral healthcare operations software can support a wide range of care settings and service models, especially where coordination, compliance, and efficiency directly impact care delivery. It is particularly valuable for:
Behavioral Health Clinics And Outpatient Practices
- Streamlines intake, scheduling, documentation workflows, and follow-ups
- Improves appointment throughput while supporting continuity of care
Group Practices And Multi-Provider Clinics
- Enables shared calendars, role-based access, standardized workflows, and workload visibility
- Reduces scheduling conflicts and administrative overhead across teams
Addiction Treatment And Recovery Centers
- Supports structured programs like detox, residential, IOP, and group sessions
- Helps manage referrals, care plans, documentation requirements, and billing workflows more consistently
Community Mental Health Organizations
- Helps coordinate high-volume caseloads, multidisciplinary teams, and community-based services
- Simplifies reporting and compliance needs tied to public funding and payer requirements
Multi-Location Providers And Growing Networks
- Standardizes operations across sites while allowing site-level flexibility
- Improves capacity planning, utilization tracking, and cross-location scheduling
Residential, Partial Hospitalization, and Program-Based Care Facilities
- Supports capacity and resource planning, structured scheduling, and program tracking
- Strengthens documentation oversight, audit readiness, and operational visibility
Common Mistakes Organizations Make When Selecting Operations Software
Several common missteps can hurt adoption and long-term value:
- Choosing a generic healthcare platform that does not match behavioral health workflows
- Focusing on feature checklists instead of day-to-day usability and workflow fit
- Leaving clinicians out of evaluation and testing, leading to resistance later
- Underestimating implementation, training, and change management
- Ignoring integration and data migration needs, creating duplicate work
Avoiding these mistakes helps organizations select software that teams actually use and trust.

The Value Of Custom Software Development in Healthcare
Standard platforms address common needs, but behavioral healthcare organizations often require tailored solutions.
Custom development becomes valuable when care models are unique, workflows span multiple programs or locations, integration requirements are complex, or organizations want technology to adapt to their processes rather than the reverse.
A healthcare-focused development partner translates clinical realities into software that supports real-world care delivery. As automation expands across intake, documentation support, and analytics, organizations are increasingly exploring AI development services to improve operational efficiency while maintaining safety and governance.
Conclusion
Behavioral healthcare depends on trust, continuity, and human connection. While technology cannot replace the clinician-patient relationship, it can remove the operational friction that often takes time and energy away from care delivery.
Behavioral healthcare operations solutions are not just about efficiency. It is about creating clearer workflows across intake, scheduling, documentation, billing, compliance, and reporting so clinicians can spend less time navigating systems and more time supporting patients. The right platform reduces administrative burden, aligns with real clinical workflows, and stays flexible as care models and programs evolve.
Selecting the right operations software is both a clinical and organizational decision. Beyond features, it is worth evaluating how well the solution fits behavioral health realities and whether the team behind it understands healthcare complexity. At EvinceDev, we build healthcare solutions with a strong focus on workflow fit, security, interoperability, and scalability so that operations support clinicians instead of slowing them down. Ultimately, better operations create the conditions for better care, delivered with consistency, compassion, and confidence.